By Lauren DeSouza- Master of Public Health, Simon Fraser Public Research University – Canada
https://newdawnscounseling.com/our-providers/
Staff Research and Content Writer
© Copyright – SUD RECOVERY CENTERS – A Division of Genesis Behavioral Services, Inc., Milwaukee, Wisconsin – August 2023 – All rights reserved.
Your risk of developing depression at some point in your life is influenced by where you live.
A new report from the Centers for Disease Control (CDC) analyzed results from the 2020 Behavioral Risk Surveillance Study and found stark differences in rates of self-reported depression across US states and counties. Hawaii had the lowest rate of self-reported lifetime depression at 12.7%, while West Virginia’s was more than double at 27.5%.
Nearly one in five US adults report being diagnosed with depression at some point in their lives. Depression has enormous health, social, and economic costs on both an individual and a societal level. Having depression reduces one’s quality of life, increases physical health conditions, and increases their utilization of health and social services. People with depression may experience loss of employment or reduced work productivity, affecting their financial status as well as the broader economy. Depression also increases social isolation and raises one’s risk of suicide and early mortality.
This study offers insight into where the burden of depression is highest. This information can inform resource allocation and program development to help state and federal programs better prevent and manage depression.
Who is most at risk of depression?
The states and counties with the highest prevalence of lifetime depression were in the Appalachian region, the southern Mississippi Valley region, and Missouri, Oklahoma, and Washington. Hawaii and California had the lowest Borough, Alaska, had the lowest county prevalence rate at 10.7%, while Logan County, West Virginia, had the highest at 31.9%.
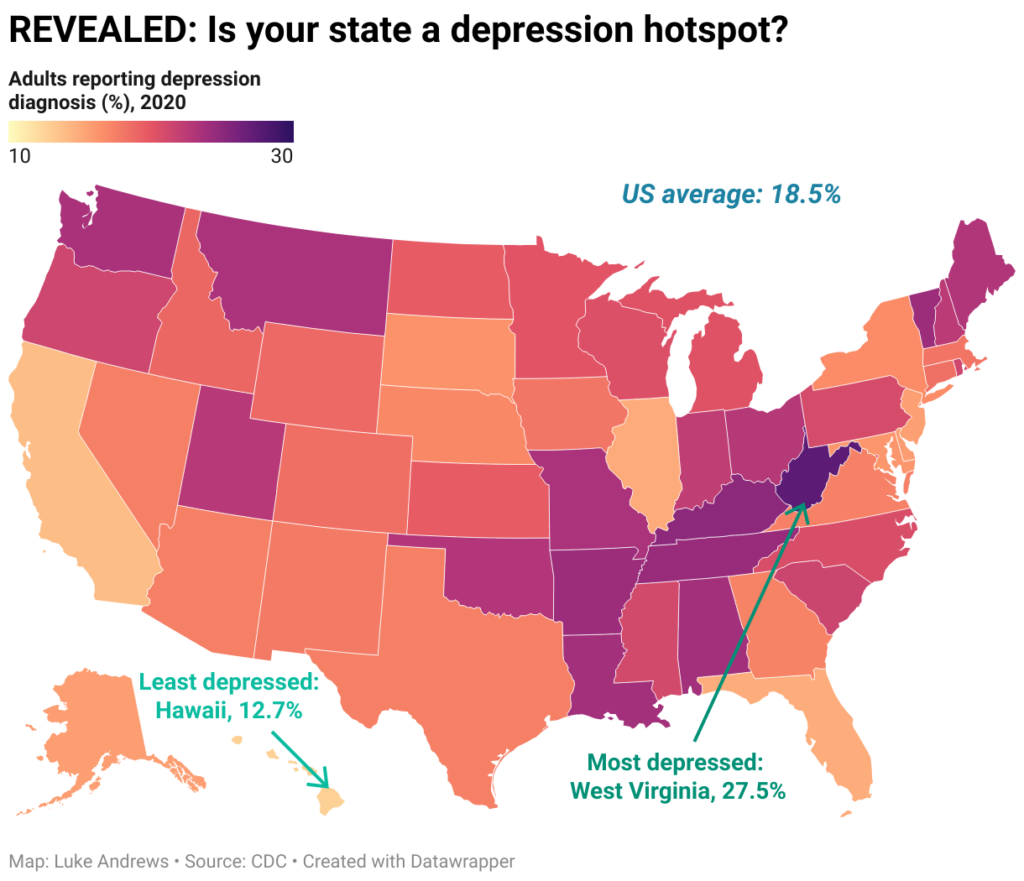
Image credit: Daily Mail
There are nuances in these data beyond the differences in prevalence among states. Specific demographics have higher rates of depression than others. For example, depression was higher among those aged 18-24 compared to those over 65, among women compared to men, and among White individuals compared to various communities of color (non-Hispanic Black, Pacific Islander, Hispanic or Latino, and Asian). Prevalence was also higher among those with lower educational attainment. Adults with less than a high school education had a higher prevalence of depression (21.2%) compared to those with a high school education or equivalent (18.5%) and a college degree or higher (15.4%).
Perhaps unsurprisingly, prevalence is highest among the 18-24 age group. Findings from the 2021 Youth Risk Behavior Survey underscore that youth mental health has worsened over the past decade; we are in the midst of a youth mental health crisis. As discussed in a previous article, the COVID-19 pandemic and resulting economic uncertainty have significantly contributed to the ongoing stress experienced by America’s youth.
Why do rates vary across states?Why are they so high in certain states?
Mental health is multifaceted and overlaps with co-occurring health issues and the social determinants of health. The social determinants of health (SDH) are the conditions and factors in the social, economic, and physical environments in which people are born, live, work, and age. These determinants play a crucial role in shaping a person’s health outcomes and well-being throughout their life. SDHs include socioeconomic status, level of education, physical environment, access to healthcare, and more. For example, those with higher poverty rates are under more chronic stress, which can contribute to health issues such as high blood pressure and diabetes. They also lack easy access to health services, a critical factor in preventing chronic diseases. Thus, the intersection of many SDHs creates conditions for chronic diseases to thrive.

Photo by Inzmam Khan on Pexels
Furthermore, depression is a comorbidity for chronic diseases, including diabetes, arthritis, and cardiovascular diseases. Those with these chronic conditions are at a higher risk of developing depression for a myriad of reasons, including stress, social isolation, and financial struggles.
The CDC report notes that those living in the Appalachian region tend to have lower incomes, higher poverty rates, and lower education levels. The aforementioned chronic conditions also occur at higher rates in these regions. Together, these factors create the conditions for the higher rates of depression reported in this geographic region.
Conversely, one would assume that Hawaii, having the lowest reported prevalence of depression, would have a very different landscape of chronic disease. The report does not discuss corresponding SDHs in Hawaii, but data from the National Center for Health Statistics from 2017 shows that Hawaii indeed has significantly fewer deaths from various chronic diseases than the rest of the US. Hawaii ranked 48th out of 50 states for the number of deaths from diabetes, heart disease, and cancer, meaning it had the 48th least number of deaths from those chronic conditions. Given the hypothesized relationship between these conditions and diabetes, one can infer that the lack of chronic disease mortality plays a role in protecting Hawaiians from depression. More research into the factors that protect those living in Hawaii from developing chronic diseases and thus depression may provide insights to improve the health of people in mainland states.
How can we make use of these results?
This report will inform data-driven decision-making to address the rise of depression in the most vulnerable states and among populations found to be most at risk. Programs include those to treat and mitigate depression (e.g., helping patients to manage their depression) and preventive measures not only in the sphere of mental health but in chronic disease prevention and management. Depression results from a domino effect of the social determinants of health and the conditions that lead to the development of chronic diseases; thus, prevention and proper management of chronic diseases are crucial to prevent depression.
The report highlights the importance of using this data to inform decision-making and prioritize health planning and interventions in areas with the greatest gaps or inequities. Evidence-based interventions recommended by organizations like The Guide to Community Preventive Services Task Force (CPSTF) and the Substance Abuse and Mental Health Services Administration (SAMHSA) could be implemented to address depression effectively.
What are the key takeaways?
- Certain states have higher rates of lifetime diagnosis of depression than others.
- Hawaii had the lowest prevalence of lifetime depression, while West Virginia had the highest.
- The social determinants of health heavily influence one’s risk of depression and are poorer in West Virginia and the surrounding Appalachian states. Chronic diseases are also more prevalent in these states and are tied to the risk of developing depression.
- Programs to prevent and treat depression in the most affected states should prioritize chronic disease prevention and management. Addressing and improving the social determinants of health is also critical to reduce depression rates.
References
Daily Mail. Depression is worst in West Virginia with more than a QUARTER reporting a lifetime diagnosis – while Hawaii has the lowest rate, CDC study reveals. June 16, 2023. Accessed from: https://www.dailymail.co.uk/health/article-12203895/Depression-worst-West-Virginia-QUARTER-reporting-lifetime-diagnosis.html
Lee B, Wang Y, Carlson SA, et al. National, State-Level, and County-Level Prevalence Estimates of Adults Aged ≥18 Years Self-Reporting a Lifetime Diagnosis of Depression — United States, 2020. MMWR Morb Mortal Wkly Rep 2023;72:644–650. DOI: http://dx.doi.org/10.15585/mmwr.mm7224a1
National Center for Health Statistics. Stats of the State of Hawaii. Updated April 13, 2018. Accessed from: https://www.cdc.gov/nchs/pressroom/states/hawaii/hawaii.htm
